Martedì 09 Aprile 2024 09:00 / Scritto da Redazione / Categoria Newsletter
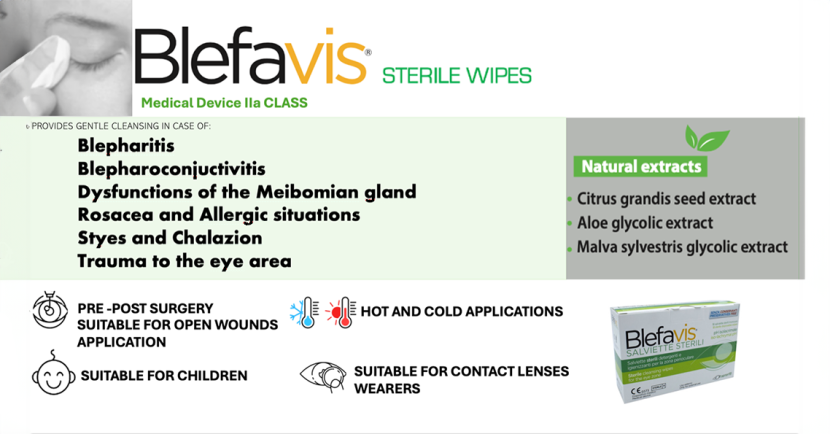
BLEFAVIS STERILE WIPES : NEW indications for children and Hot&Cold applications.
Eyelids consist of thin folds of skin, muscle, and connective tissue. They protect the eyes and spread tears over the front of the eyes. The inside of the eyelids are lined with the conjunctiva which is called the palpebral conjunctiva. The outside of the lids are covered with the body’s ...
Eyelids consist of thin folds of skin, muscle, and connective tissue. They protect the eyes and spread tears over the front of the eyes. The inside of the eyelids are lined with the conjunctiva which is called the palpebral conjunctiva. The outside of the lids are covered with the body’s thinnest skin.
Eye lid inflammations include mainly stye, blepharitis, chalazion:
- A stye is an infection of one of the three types of eyelid glands near the lid margins, at the base of the lashes. The result is a painful lump on the edge of your eyelid. A stye is usually most visible on the surface of the eyelid. A stye is a bacterial infection (staphylococcus aureus) involving one or more of the small glands near the base of your eyelashes. It is similar to a boil or a pimple and is often painful.
- A chalazion is an enlargement of a meibomian gland which is an oil-producing gland in the eyelid. A chalazion occurs when there’s a blockage in one of the small oil glands at the margin of the eyelid, just behind the eyelashes. This blockage causes inflammation of the gland, which makes the eyelid swell and redden. This is usually not associated with an infectious agent. More likely, the gland opening is clogged. Initially, a chalazion may resemble a stye, but it usually grows larger. A chalazion may also be located in the middle of the lid and be internal. Although a chalazion can be painful when developing, it can become a relatively painless swelling that feels like a small bead in your eyelid.
- Blepharitis is the inflammation of the eyelid margins, often with scales and crust. It can lead to itchiness, red eyes, greasy and crusted eyelids, eyelash loss, ectropion, corneal damage, excessive tearing, and chronic conjunctivitis. Some cases of blepharitis are caused by bacterial infection, but in some cases, the cause is unclear: Seborrheic dermatitis — dandruff of the scalp and eyebrows Infection, Clogged or malfunctioning oil glands in your eyelids, Rosacea — a skin condition characterized by facial redness, Allergies, including allergic reactions to eye medications, contact lens solutions or eye makeup, Eyelash mites or lice, Dry eyes. It may also be caused by an overproduction of oil by the meibomian glands. Blepharitis can be a chronic condition that begins in early childhood and can last throughout life.
Incidence of eye lid inflammation is 1.8 per 1000 per year. It accounts for 4.5% of all ophthalmological problems. Blepharitis is the most common ocular disease known.
Good lid hygiene is very important. Regular eyelid washing with baby shampoo or special lid scrub helps prevent styes, chalazia, blepharitis, and eyelid edema. To avoid these problems, it’s also important to refrain from touching and rubbing the eyes and eyelids, especially with hands that have not just been washed.
What are the types of blepharitis?
To better understand this condition, think of the eyelid as being composed of two layers, one in front of the other. Each of these layers contains unique structures whose function may be affected by blepharitis.
- Anterior blepharitis is related to inflammation of the front layer of the eyelid. The symptoms usually are limited to ocular itching, burning and irritation. Although there are many possible causes of anterior blepharitis, it is most often related to bacterial infection or seborrheic dermatitis, a chronic inflammatory skin condition. Seborrheic dermatitis is a common problem affecting the scalp, eyebrows, face and eyelids in two-thirds of anterior blepharitis patients. It is the most common cause of blepharitis. This condition leads to oily secretions, eyelid swelling, scaling and flaking produce ocular itching and burning that can be severe. Both layers of the eyelid may be affected.
- Posterior blepharitis occurs when the small (meibomian) glands in the inner layer of the eyelid either become inflamed or secrete an excessive quantity of their normal product. These glands produce an oily substance, an important part of the normal tear film that bathes the surface of the eye. Overproduction of this substance can produce a bothersome burning sensation of the eyes, although the eyelids may remain normal in appearance. In contrast, patients suffering from gland inflammation may also complain of a burning sensation as well as tearing, itching, irritation, sensitivity to light and crusting upon awakening in the morning. In these patients, the eyelid margin may appear red and swollen. The cause of gland inflammation is unknown, but bacterial infection or plugging of the glands by abnormally thick secretions is thought to play a role.

The treatment of periocular inflammations
The cornerstone of therapy is good eyelid hygiene:
- Styes are treated with warm compresses for 10-15 minutes, three to four times a day. Sometimes topical antibiotics may be prescribed if the infection is spreading. Occasional blurriness may occur after eyedrops or ointments are placed in your eyes. This should clear up quickly.
- One fourth of chalazia will disappear spontaneously, but warm compresses may speed the process. Because chalazia are inside the lid, topical medications are generally of no benefit.
- Blepharitis is treated with hot compresses, with antibiotic ointment, and by cleaning the eyelids with a moist washcloth and then with baby shampoo. Good hygiene is essential. Tear film supplements can help moisten the eyes when dry. Topical or systemic antibiotics also may be prescribed. If the blepharitis doesn’t clear up with treatment or if it seems to be a chronic problem, the patient may have acne rosacea. These patients may need to see a dermatologist as well.
- Blepharitis is a chronic condition. Treatment involves thorough eyelid cleansing aimed at keeping the eyelid margin free from crusts and secretions. Both anterior and posterior blepharitis are treated with warm compresses (warm, moist wash cloth applied to the eyelid) followed by lid cleansing (using a moist cotton swab to gently clean the eyelid margin) two to three times each day. For posterior blepharitis with significant meibomian gland dysfunction, some physicians may recommend treatment with oral antibiotics. Blepharitis is a difficult disease to treat and a complete cure is not easily achieved. Effective treatment requires a long-term commitment from both patient and physician.
Who can get blepharitis?
Adults are affected more often than children. The condition may occur at an increased frequency within certain families and in children with Down’s syndrome. Multiple studies have shown that the onset of eyelid inflammations in the pediatric setting is typically between 3 and 5 years of age; however, the diagnosis is often delayed 1 to 3 years, due to a high frequency of missed diagnosis or misdiagnosis. In children, the true incidence and prevalence is controversial; however, 1 study reports that eyelid inflammations are the reason for referral to pediatric ophthalmology in 12% to 15% of cases. Children of Asian descent may be the most affected, while children of Indo-Pakistani and Middle Eastern descent often have more severe presentations.Eyelid margin disease is also common in the general population; 1 survey of US ophthalmologists and optometrists reported that 37% and 47% of all patients seen by those surveyed, respectively, had evidence of blepharitis. Infantile seborrheic dermatitis (ISD) is a chronic, inflammatory scaling skin condition in infants and young children that presents with a greasy, patchy rash typically affecting the scalp (referred to as cradle cap, or formally Pityriasis capitis), eyebrows, or skin folds of the neck, arms, or diaper areas. A large study from Australia showed a high prevalence of seborrheic dermatitis in 44.5% of children younger than 12 months.
Blefavis sterile wipes: hot&cold applications and e pediatric use
The formulation of the product BLEFAVIS STERILE WIPES is based on the following components which have detergent and emollient characteristics, and lead to normalization of the presence of bacteria on the skin.
- G.S.E standardized extract (grape seed extract),
- Standardized extract of Aloe,
- Standardized extract of Malva Silvestris
The BLEFAVIS sterile periocular wipes medical device has undergone a stability study to make a change to the instructions for use of the medical device which consists in the inclusion of the possibility of storing the wipe in the fridge or heating it in a bain-marie at approximately 40°C before use.
The stability study was carried out at the Department of Chemical, Pharmaceutical and Agricultural Sciences of the University of Ferrara in the period May – June 2023.
On the basis of the results obtained we can conclude that BLEFAVIS sterile periocular wipes are stable and maintain their quality specifications both after repeated temperature changes from 25 °C to 4 °C and vice versa and after heating at 40 °C even for prolonged periods.
The results of the study allow us to include in the instructions for use the possibility of storing and using the wipe in the fridge or heating it in a bain-marie at approximately 40°C before use, also as an additional efficiency on the cleansing of the periocular area:
“In case of particularly persistent secretions and/or occlusion of the tear duct, it is advisable to heat the sealed sachet for a few minutes in warm water (about 40°C) and then use the towel as a warm compress, massaging gently. In case of inflammation it is advisable to cool the closed sachet in the refrigerator for a few hours and then apply the open towel on the eye, keeping it for a few minutes as a cold compress”.
Another observational study aimed to evaluate how the use of a specific medical device for eyelid hygiene, BLEFAVIS STERILE WIPES. prescribed individually or combined with pharmacological therapy, allows a quicker resolution of the ongoing problem, even from children of 4 years of age
The patients who were selected for the study, from 4 years old of age, showed BLEPHARITIS, CHALAZIO and STAY
At the end of this observational study, it was possible to see how by using a specific product for eyelid hygiene the symptoms reported by patients, from children of 4 years of age, were significantly reduced or disappeared more quickly compared to the control group and also the therapy combined with eyelid hygiene showed greater effectiveness, with better results in less time.
In pediatric use, it was possible to deduce a great help in eliminating the symptoms in relation to cleansing with traction on the dermis to clean any crusts present.
The use of Blefavis Sterile Wipes has demonstrated maximum effectiveness in significantly reducing the symptoms of the pathologies described, as well as highlighting a great tolerability and comfort.
—


